What is Ankylosing Spondylitis?
- Grace. T

- Sep 26, 2025
- 4 min read

Ankylosing Spondylitis: The Spine’s Silent Battle
Introduction
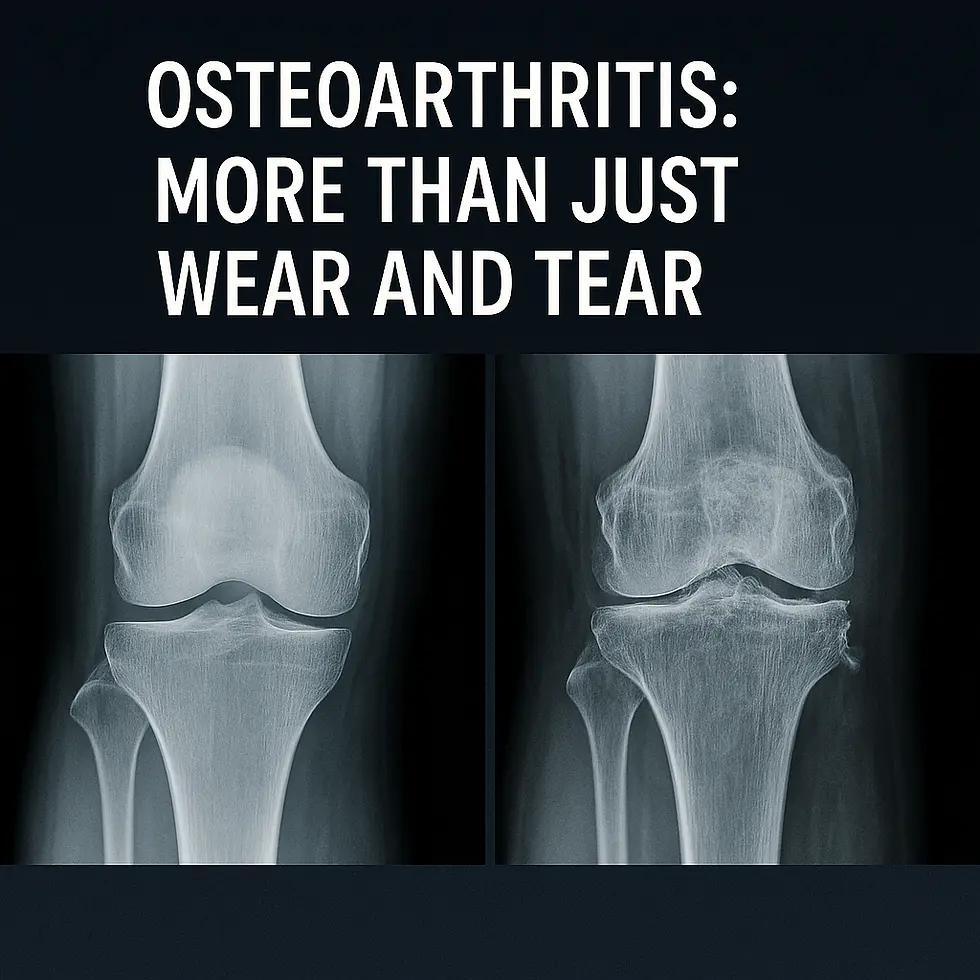
Ankylosing Spondylitis (AS) is a chronic inflammatory arthritis that primarily affects the spine and sacroiliac joints (where the spine meets the pelvis). Unlike osteoarthritis, which develops from “wear-and-tear,” AS is an autoimmune condition — meaning the body’s immune system mistakenly attacks its own tissues, causing inflammation. Over time, this inflammation can lead to new bone formation, causing the spine to stiffen or even fuse, resulting in reduced flexibility and a forward-stooped posture.
AS is often underdiagnosed because its earliest symptoms look like common back pain. However, it typically starts in younger adults (late teens to early 30s), not in older adults where degenerative arthritis is more expected. Early recognition is critical for maintaining quality of life.
Why This Matters for Nursing Students
For nursing students — and healthcare providers in general — AS teaches an important lesson: not all back pain is the same.
Most people think of back pain as mechanical (lifting heavy objects, poor posture, strain), but AS is inflammatory. Patients often describe a pattern that’s opposite of mechanical pain:
Inflammatory pain: Worse in the morning or after rest, improves with exercise.
Mechanical pain: Worse with movement, improves with rest.
This makes lifestyle counseling vital. Many patients fall into the cycle: “I hurt because I don’t move, I don’t move because I hurt.” Understanding this cycle helps nurses encourage safe movement and prevent disability.
Signs and Symptoms (Explained)
Chronic low back pain & stiffness: Typically lasting more than 3 months. Inflammation in the sacroiliac joints causes pain deep in the buttocks and lower spine.
Morning stiffness: Patients often wake up with a stiff back that improves once they start moving. This is a hallmark of inflammatory arthritis.
Fatigue: Chronic inflammation produces inflammatory chemicals (like TNF-alpha) that drain energy levels.
Decreased spinal mobility: As the disease progresses, the vertebrae can fuse, limiting bending, twisting, and chest expansion.
Forward-stooped posture: In advanced cases, spinal fusion forces the patient into a hunched position that cannot be straightened.
Other organ involvement: Some patients develop uveitis (eye inflammation), restricted lung function, or bowel inflammation (associated with Crohn’s disease or ulcerative colitis).
Lifestyle Factors and Triggers
Modern lifestyles can worsen AS symptoms:
Prolonged sitting (desks/keyboards/screens): Lack of spinal movement increases stiffness and pain. Sedentary workers (IT professionals, office staff, students) are at higher risk of worsening symptoms.
Poor posture: Hunching forward over devices accelerates spinal rigidity.
Sedentary habits: Without daily stretching, joints lose flexibility.
This is why physiotherapy and daily activity are considered as important as medications in treatment.
I hurt because I don’t move, and I don’t move because I hurt.

Nurses play a key role in helping patients manage AS through education and support:
Patient education: Explain the difference between mechanical and inflammatory pain. Many patients don’t realize that moving can help reduce pain.
Exercise promotion: Recommend safe, low-impact activities like swimming, yoga, or walking. These strengthen muscles, preserve flexibility, and reduce stiffness.
Ergonomics: Encourage patients to use adjustable chairs, standing desks, and lumbar support.
Monitoring complications: Reduced chest expansion means patients are more prone to breathing issues; eye pain may indicate uveitis, which needs immediate attention.
Psychological support: Living with chronic pain can lead to frustration, depression, and social withdrawal. Nurses can support coping strategies and connect patients with resources.
Home Treatment and Self-Care
Daily stretching: Gentle spinal mobility exercises can prevent stiffness and improve function.
Heat therapy: Warm showers, heating pads, or hot baths ease morning stiffness.
Cold packs: Used for acute pain flare-ups.
Sleep hygiene: Supportive mattresses and proper pillows keep the spine aligned.
Lifestyle: Quitting smoking improves lung capacity and reduces complications.
Pacing activities: Patients should stay active but avoid overexertion, balancing rest with movement.
Conclusion
Ankylosing Spondylitis is more than “just back pain” — it’s a lifelong inflammatory condition that challenges patients physically and mentally. For nursing students and healthcare providers, understanding AS means looking beyond the obvious, identifying patterns of inflammatory pain, and addressing the cycle of immobility that so often traps patients.
By combining education, empathy, and practical interventions, nurses can empower patients to maintain mobility and independence despite the challenges of living with AS.
Case Scenario
A 29-year-old IT professional reports morning stiffness, worsening lower back pain after long hours at their desk, and relief after exercise. They state: “I hurt because I don’t move, and I don’t move because I hurt.”
Questions for Nursing Students:
What condition should you suspect based on these symptoms?
A) Osteoarthritis
B) Ankylosing Spondylitis
C) Rheumatoid Arthritis
D) Gout
What lifestyle advice would you give this patient to manage symptoms?
A) Rest as much as possible
B) Avoid exercise to reduce strain
C) Engage in daily stretching and low-impact activity
D) Increase desk work to “push through” the pain
ANSWERS AT BOTTOM OF POST - How did you do?
💡 Ready to Get Certified?
Be prepared. Be confident. Learn First Aid Today & Save a Life Tomorrow with Saving Grace Medical Academy Ltd. Now enrolling: Basic Life Support (BLS) & Standard First Aid CPR-C & AED courses designed for healthcare professionals.
📍 Training for First-Year Nursing Students
Join Saving Grace Medical Academy Ltd. for fully certified, CSA-compliant Standard First Aid CPR-C & AED courses—designed for Alberta’s future healthcare professionals.
Just Remember:
Protect Yourself. Call 911.Don’t Waste Time.
RESOURCES:

Author - Saving Grace Medical Academy Ltd
Grace. T
Medical Content Writer
Answers & Explanations
B) Ankylosing Spondylitis → Young age, chronic low back stiffness improving with activity, and sacroiliac pain are classic signs of AS.
C) Engage in daily stretching and low-impact activity → Movement relieves stiffness and prevents progression, whereas rest alone worsens symptoms.