What is Osteoarthritis?
- Grace. T

- Sep 18, 2025
- 4 min read
Updated: Sep 19, 2025
Understanding Osteoarthritis: What Nursing Students Need to Know
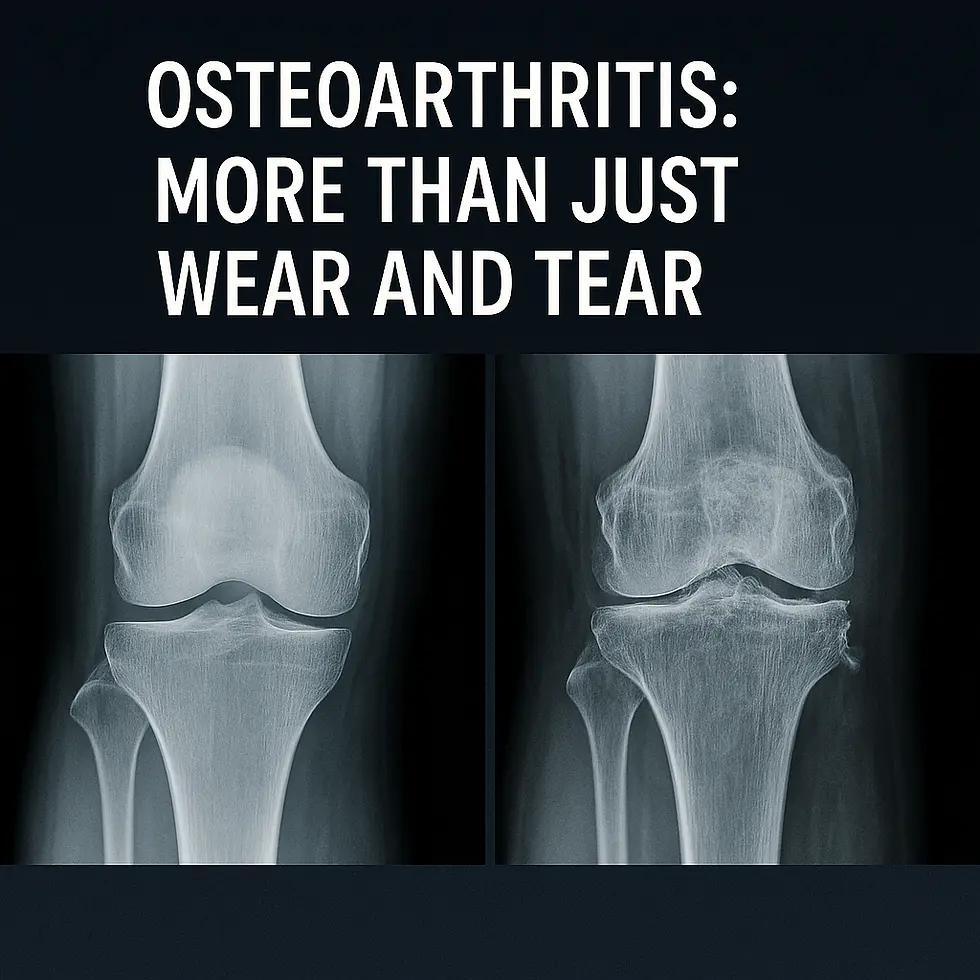
What is Osteoarthritis? Osteoarthritis (OA) is the most prevalent form of arthritis, affecting millions worldwide. Unlike autoimmune conditions such as rheumatoid arthritis, OA is a degenerative joint disease caused by the gradual breakdown of cartilage. Nursing students will encounter OA frequently in clinical practice, especially in older adults, making it essential to understand its causes, risk factors, symptoms, and management.
Causes and Risk Factors
Osteoarthritis occurs when the protective cartilage that cushions the ends of bones wears down over time. This leads to friction, pain, and joint damage.
Key Risk Factors Include:
Age: Risk increases with age.
Gender: Women are more likely to develop OA, particularly after menopause.
Joint Injury: Previous fractures or injuries can accelerate cartilage breakdown.
Obesity: Excess body weight adds stress to weight-bearing joints like the hips and knees.
Genetics: Family history can predispose individuals.
Why this is important: Nursing students must recognize that OA is not just “wear and tear.” Risk factors like obesity or past injuries highlight the importance of patient education on prevention and lifestyle management.
Symptoms and Clinical Presentation
Osteoarthritis develops gradually and worsens over time. Common symptoms include:
Joint pain during or after movement
Stiffness, particularly in the morning or after inactivity
Swelling around affected joints
Decreased range of motion
Grating or popping sensation (crepitus)
Why this is important: Recognizing early signs of OA helps nurses advocate for timely interventions, preventing unnecessary disability and improving patient quality of life.

Treatment and Management
While OA has no cure, treatment focuses on symptom relief and maintaining joint function.
Non-Pharmacological Approaches:
Weight loss to reduce stress on joints
Physiotherapy and regular exercise (low-impact activities such as swimming or cycling)
Joint protection techniques (braces, supportive footwear)
Pharmacological Approaches:
Acetaminophen or NSAIDs for pain relief
Corticosteroid injections for severe inflammation
Surgical Interventions:
Joint replacement (hip, knee) in advanced cases
Home Treatment and Self-Care for Osteoarthritis
In addition to medical treatment, patients with osteoarthritis can benefit from lifestyle changes and self-care strategies to manage symptoms and maintain independence:
Exercise: Low-impact activities like walking, swimming, and cycling strengthen muscles around joints, improve flexibility, and reduce stiffness.
Weight management: Even a modest weight loss can decrease joint stress, especially in the knees and hips.
Heat and cold therapy:
Heat (heating pads, warm baths) helps reduce stiffness.
Cold packs relieve joint swelling and acute pain.
Assistive devices: Braces, splints, or canes can support joints and reduce strain.
Joint protection: Encourage pacing activities, using proper body mechanics, and avoiding repetitive stress on affected joints.
Healthy diet: A balanced diet rich in anti-inflammatory foods (fruits, vegetables, omega-3s) may help reduce overall joint inflammation.
Note for nursing students: Educating patients about at-home care improves quality of life, reduces reliance on medications, and empowers patients to take an active role in their condition management.
Why this is important: Nurses play a central role in teaching patients self-management strategies, monitoring pain control, and supporting recovery from surgical interventions.

Case Scenario for Nursing Students
A 68-year-old woman presents with chronic knee pain that worsens with walking and improves with rest. She reports stiffness in the morning lasting less than 30 minutes and occasional swelling after activity. Her BMI is 32.
Questions for Review:
What risk factors for OA does this patient present with?
A) Obesity and age
B) Family history and infection
C) Gender and trauma history
D) Rheumatoid factor positivity
Which non-pharmacological intervention would you recommend first?
A) High-impact aerobics
B) Swimming or cycling
C) Immediate joint replacement
D) Daily corticosteroid injections
ANSWERS AT BOTTOM OF POST - How did you do?
💡 Ready to Get Certified?
Be prepared. Be confident. Learn First Aid Today & Save a Life Tomorrow with Saving Grace Medical Academy Ltd. Now enrolling: Basic Life Support (BLS) & Standard First Aid CPR-C & AED courses designed for healthcare professionals.
📍 Training for First-Year Nursing Students
Join Saving Grace Medical Academy Ltd. for fully certified, CSA-compliant Standard First Aid CPR-C & AED courses—designed for Alberta’s future healthcare professionals.
Just Remember:
Protect Yourself. Call 911.Don’t Waste Time.
RESOURCES:

Author - Saving Grace Medical Academy Ltd
Grace. T
Medical Content Writer
Answers & Explanations
1) What risk factors for OA does this patient present with?
✅ A) Obesity and age
Why: She’s 68 years old (age is a major OA risk) and has a BMI of 32 (excess load on weight-bearing joints).
Why not B: No history of infection is given.
Why not C: Gender (female) does increase risk post-menopause, but trauma history isn’t mentioned.
Why not D: Rheumatoid factor is associated with RA, not OA, and isn’t part of the case.
2) Which non-pharmacological intervention would you recommend first?
✅ B) Swimming or cycling
Why: These are low-impact activities that reduce joint load while building strength and improving function—first-line for knee OA.
Why not A: High-impact aerobics can worsen pain and joint stress.
Why not C: Joint replacement is reserved for advanced, refractory cases after conservative measures.
Why not D: Daily corticosteroid injections are inappropriate; injections (when used) are intermittent and not first-line.







