Lead Poisoning
- Jason T

- Aug 14, 2025
- 8 min read
Updated: Aug 20, 2025

Lead Poisoning: What Is It?
Definition & Overview: Lead poisoning occurs when lead—a colorless, tasteless, odorless heavy metal—accumulates in the body over time, typically via inhalation or ingestion. Even small exposures can become hazardous, especially with repeated or chronic contact.
Why It Matters Understanding the stealthy onset of lead poisoning is crucial for nursing students—early identification can protect patients before irreversible damage occurs.
Lead Exposure and the “Golden Age of Serial Killers”
The 1970s and 1980s are often referred to as the “Golden Age of Serial Killers,” a time when notorious offenders such as Ted Bundy, John Wayne Gacy, and David Berkowitz dominated headlines. This period also coincided with peak global use of leaded gasoline, lead-based paints, and emissions from lead smelters—resulting in unprecedented environmental contamination. Research has shown that chronic lead exposure, especially in childhood, can cause neurological damage leading to increased aggression, impulsivity, and reduced empathy—traits that could amplify violent tendencies in predisposed individuals. While this does not prove lead was the sole cause behind the psychological makeup of serial offenders, the overlap between peak environmental lead exposure and the rise in violent crime rates during the 20th century has been compelling enough for criminologists, neuroscientists, and public health researchers to investigate the connection. Importantly, violent crime rates began to drop significantly in the 1990s—roughly 20 years after the U.S. and other nations began phasing out leaded gasoline, aligning with the timeframe it would take for lead exposure levels in children to decline.
Author and Personal Researcher: Caroline Fraser looks into the connection of Lead Exposure and the creation of serial killers in her book: Murderland Crime and Bloodlust in the Time of Serial Killers where she uncovers the connections of Lead exposure and personality disorders in the 1970's.
What Causes Lead Poisoning?
Lead exposure stems from various environmental and occupational sources, including:
Older homes (lead-based paint, plumbing)
Drinking water via lead solder or pipes
Ammunition, weights, batteries
Hobbies needing solder, glazed pottery, art supplies
Why It Matters Nurses must assess environmental and lifestyle factors when evaluating patients—knowing common lead sources helps in accurate diagnosis and prevention counseling.

How Does Lead Damage the Body (and Mind)?
Physical Effects: Lead mimics essential minerals and accumulates in bones, disrupting red blood cell production (causing anemia), and impairing calcium absorption affecting neuromuscular and vascular function:
Cognitive & Mental Effects
In children, even low blood lead levels (< 5 µg/dL) can reduce IQ by 3–5 points, impair executive function, and cause learning and behavioral problems (e.g. ADHD)
Adults exposed in childhood often show higher rates of neuroticism, lower conscientiousness and agreeableness—traits impacting long-term mental health, socio-economic outcomes, and personal relationships
Elevated lead exposure is correlated with increased aggression, impulsivity, and even violent behavior in adulthood
One study attributes over 150 million mental health disorder cases (ADHD, anxiety, depression) to historical lead exposure from gasoline in people born 1966–1986
Moreover, secondary personality changes—termed "organic personality disorder"—can occur due to lead-induced brain injury, resulting in emotional instability, disinhibition, apathy, paranoia, or personality shifts.
Why It Matters For nursing students, it's critical to recognize that lead poisoning is not solely a physical or pediatric issue—it can manifest through complex psychiatric symptoms and personality changes. This awareness enhances holistic patient care and interdisciplinary collaboration.
Alberta, Canada — Legacy of Lead in Water Pipes
Historical Use of Lead in Plumbing
In Alberta, lead service lines were widely installed in municipal water systems until approximately 1975, and solder containing lead was used in plumbing and repairs until about 1986. Additionally, brass and bronze fittings could still contain lead until 2013
As a result, homes built before 1960 are particularly susceptible to having lead in their service lines, internal plumbing, solder, or fixtures
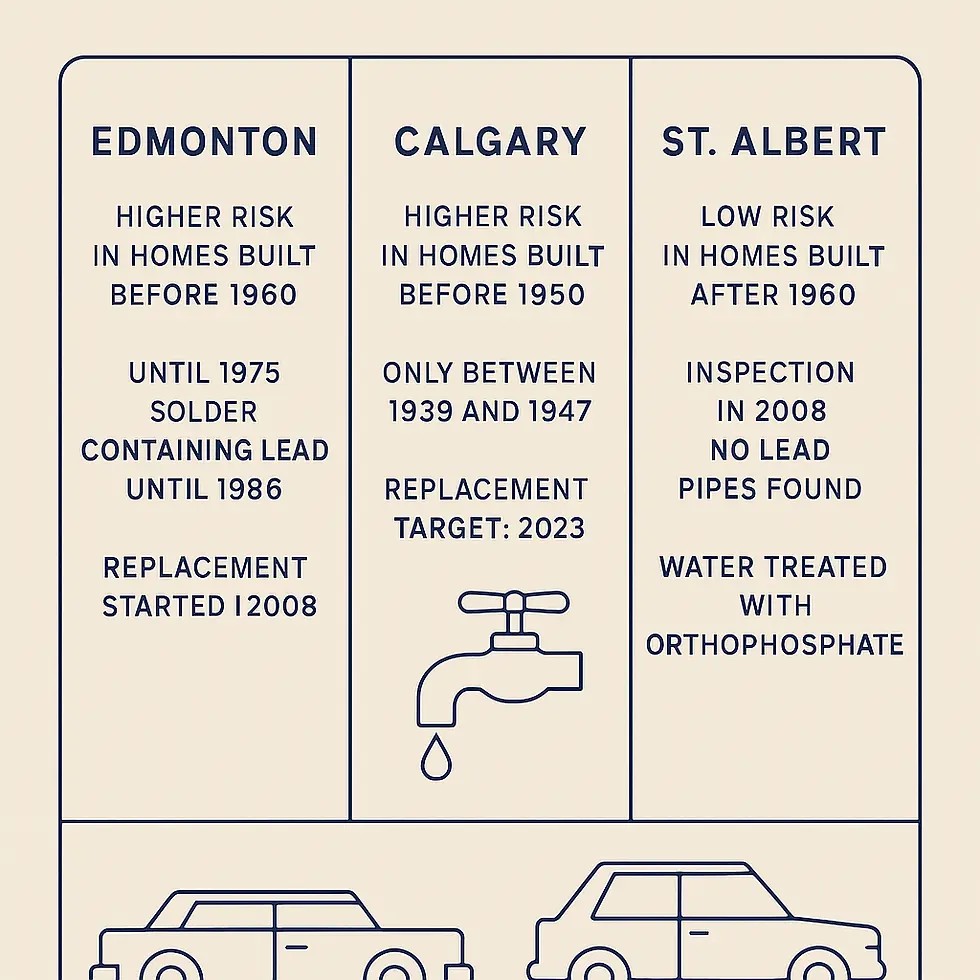
City-by-City Snapshot: What Nursing Students Should Know
Edmonton
Edmonton’s utility provider, EPCOR, acknowledges this legacy and has been proactively replacing lead service lines since 2008
EPCOR’s lead management program includes:
Annual notifications to affected households
Free water testing at the tap
Provision of point-of-use filters
Coordination of utility-side pipe replacements
Homeowners remain responsible for their portion of the service line—from property line to meter—not reliably documented by EPCOR
Calgary
In Calgary, lead service connections were only used briefly between 1939 and 1947, mainly due to copper shortages during World War II
The City of Calgary’s accelerated lead service line removal plan, approved in October 2020, set a goal to replace remaining lead service lines by 2023, funded by a cost-sharing model ($14M city; $2.5M via utility rates)
Many older residential service lines remain unclassified; the city launched efforts in 2020 to identify materials in homes built before 1950
St. Albert
In contrast, St. Albert—where most homes were built after 1960—has a very low risk of lead service lines.
Inspections conducted in 2008 on homes built before 1960 found no lead pipes
As of 2023, St. Albert’s water utility supplies water treated with orthophosphate (a corrosion inhibitor), helping to further reduce lead leaching risks
Clinical Impact on Children & Adults
Children
Developmental delays: learning disabilities, lower IQ, ADHD, behavioral issues, hearing loss, growth stunting, seizures, and in severe cases, coma or death
Adults
Symptoms include abdominal pain, muscle weakness, neurological deficits, hypertension, fertility issues, irritability, memory problems, depression, and sleep disturbances
Persistent cognitive and mental health deficits from childhood exposures may impair social functioning and increase psychiatric illness risk throughout life
Why It Matters Nurses must be prepared to identify and manage lead poisoning across the lifespan, recognizing both immediate physical signs and long-term mental health sequelae.
Prevention & Screening
No level of lead is considered safe—minimizing exposure is essential
Routine blood lead level screenings are recommended for children around 12–15 months, especially if environmental risk factors are present
Environmental assessments should consider age of housing, water plumbing, hobbies, and occupational exposures.
Why It Matters Early detection through proactive screening enables timely intervention—nursing professionals play a key role in educating families and advocating for public health measures.
Diagnosis
Blood lead level measurement is the standard diagnostic tool. Traditional thresholds (e.g., 10 µg/dL in the U.S.) are being replaced by lower reference levels as research shows harm at even minimal exposure.
Why It Matters Stay current with evolving guidelines and reference values to ensure accurate diagnosis and patient advocacy.

Treatment
Mild exposure: Remove source of lead, optimize nutrition (iron, calcium, vitamin C).
Severe exposure (≥ 45 µg/dL): Hospitalization and chelation therapy using agents to bind and eliminate lead
Long-term: Monitor cognitive, emotional, and behavioral outcomes; collaborate with mental health professionals for support when needed.
Why It Matters Treatment extends beyond lowering blood lead levels—it includes ongoing support for neurocognitive and psychiatric recovery. Nurses guide this long-term, multidisciplinary care.
Emergency Situations
In the event of acute severe toxicity—symptoms like seizures, coma, or encephalopathy—immediate emergency intervention (e.g., call 911 or local emergency services like Alberta’s Health Link at 811) is vital.
Why It Matters Triaging and emergency response skills are essential in recognizing life-threatening lead toxicity and initiating rapid treatment.
Final Thoughts for Nursing Students
Holistic understanding: Lead poisoning impacts both body and mind—nursing care must address both.
Advocacy: Promote lead-free environments and support public health initiatives targeting lead remediation.
Continuing education: Stay informed of emerging guidelines, mental health ramifications, and evidence-based interventions.
References & Further Reading
Lead's long-term mental health impact: over 150 million psychiatric cases linked to gasoline-era exposure
Cognitive, behavioral, and personality effects from childhood lead exposure
PNAS.
Organic personality disorder due to medical brain injury like lead poisoning
Cognitive and behavioral impairments even at “safe” levels of exposure
Treatment guidelines for mild vs. severe exposure
Case Scenario for Nursing Students
TEST YOURSELF
Scenario You are working in a pediatric outpatient clinic when a 7-year-old boy, Liam, is brought in by his mother. She reports he has been more irritable lately, struggling with concentration at school, and complaining of stomach aches. His teacher has also noted a drop in academic performance and increased impulsive behavior.
Physical assessment reveals:
Slight pallor
Mild abdominal tenderness
Blood pressure: 118/76 mmHg (elevated for age)
Neurological exam: No focal deficits, but mild difficulty following multi-step instructions
Laboratory results: Blood lead level = 32 µg/dL
His mother mentions they live in a rental home built in the 1950s that still has its original windows and paint.
Multiple Choice Questions
1. Based on Liam’s presentation, which of the following is the most likely primary source of his lead exposure?
A) Tap water from copper pipes
B) Lead-based paint dust from home renovation
C) Imported plastic toys
D) Pesticide exposure from gardening
2. Which of the following symptoms in Liam may be linked to lead’s neurotoxic effects?
A) Mild abdominal pain
B) Impulsivity and poor concentration
C) Pallor
D) Elevated blood pressure
3. At Liam’s blood lead level, which is the most appropriate next step in management?
A) Immediate chelation therapy in hospital
B) Identify and eliminate the lead source, provide dietary counseling, and recheck levels in 1–3 months
C) No treatment needed; monitor annually
D) Start antihypertensive medication immediately
4. Long-term follow-up for Liam should focus on which area in addition to physical health?
A) Annual cardiac stress testing
B) Monitoring for personality changes and learning disabilities
C) Regular hearing tests only
D) Limiting outdoor play
Rationale for Nursing Students
Early recognition of subtle neurobehavioral changes can prompt earlier intervention.
Holistic care includes environmental assessment, nutritional counseling, mental health monitoring, and academic support referrals.
Interdisciplinary approach involving public health, social services, and school-based resources ensures a comprehensive plan.
ANSWERS AT BOTTOM OF POST
💡 Ready to Get Certified?
Be prepared. Be confident. Learn First Aid Today & Save a Life Tomorrow with Saving Grace Medical Academy Ltd. Now enrolling: Basic Life Support (BLS) & Standard First Aid CPR-C & AED courses designed for healthcare professionals.
📍 Training for First-Year Nursing Students
Join Saving Grace Medical Academy Ltd. for fully certified, CSA-compliant Standard First Aid CPR-C & AED courses—designed for Alberta’s future healthcare professionals.
Just Remember:
Protect Yourself. Call 911.Don’t Waste Time.
RESOURCES:
Advanced Cardiovascular Life Support - Heart & Stroke Foundation
Basic Life Support BLS- CPR Course 09:00am | Saving Grace Medical
Advanced Cardiovascular Life Support Course | Saving Grace Medical
Member Update: Grande Prairie Building Lead Exposure | Health Sciences Association of Alberta
Doctors, parents warned of risks to children from low-level lead exposure | Folio
Bovine lead poisoning in Alberta: A management disease - PubMed

Author - Saving Grace Medical Academy Ltd
Jason T
Retired EMT - Heart & Stroke Foundation Senior Instructor
TEST YOURSELF - ANSWERS
Correct Answer: B – Homes built before 1978 often contain lead-based paint. Peeling or chipping paint, especially around windows and doors, can generate lead dust easily inhaled or ingested by children.
Correct Answer: B – While all listed symptoms can be seen in lead poisoning, impulsivity and poor concentration directly reflect lead’s impact on the developing brain, contributing to behavioral and cognitive deficits.
Correct Answer: B – Blood lead level of 32 µg/dL is high but below the threshold for urgent chelation therapy in most guidelines. Priority is to remove the source, optimize nutrition (iron, calcium, vitamin C), and monitor closely.
Correct Answer: B – Chronic lead exposure can result in neurodevelopmental delays, learning disabilities, ADHD-like symptoms, and personality changes. Ongoing neuropsychological support is essential.





